Ankle Sydesmosis injuries
It is timely with the 2021 AFL season commencing last week that we discuss Ankle Sydesmosis injuries. In the 2020 shortened AFL season there was a remarkable 4 fold increase in ankle syndesmosis injuries with a total of 21 injuries suffered by the likes of Jake Stringer, Dion Prestia, Toby Nankervis, Aaron Naughton and Andy McGrath.
So what is a syndesmosis injury, how are they treated and why has it become so prevalent in the modern AFL game?
Syn-des-what!?
You may be asking yourself …’the syn-des-what..?’.
Yes, Syndesmosis it is a funny name and it refers to a ligament located between the two shin bones (tibia and fibula) in the lower leg. There is little movement between the tibia and fibula due to the strength of this ligament and others around it. Damage to these ligaments leads to a loss of stability at the bottom of the shin and particularly the ankle. This often results in reduced ankle joint movement, reduced balance, stability and power. These are all key attributes an AFL player must possess with fast changes in direction, speed and repeated jumping and landing during a game.
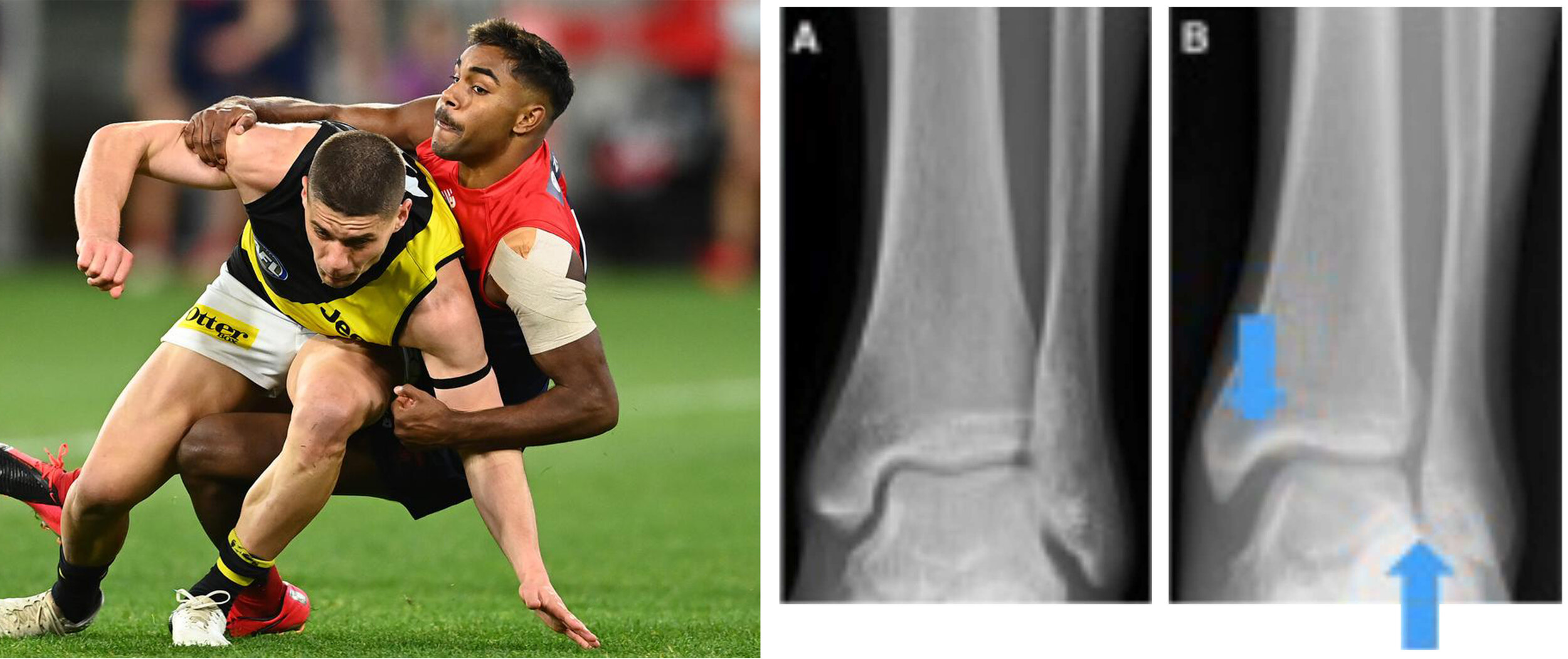
Possible long term changes in the quality of movement at the ankle joint due to this injury can likely lead to degenerative changes, such as arthritis. Syndesmosis injury is most common in contact sports, especially when landing heavily and being tangled up with another person during the landing. AFL, rugby and basketball are common sports which have increased risk.
Notice the increased width in image B between the two bones which indicates that the syndesmosis ligament has been damaged.
How is it different to a common lateral ankle sprain?
More generally the ankle has a number of ligaments and tendons that overall help stabilise the joint. Even after a severe traditional lateral ankle sprain these muscles and tendons will continue to offer some support. With the right management a traditional ankle sprain will recover without requiring any surgical intervention.
A syndesmosis injury is more commonly referred to as a ‘high ankle sprain”. They generally occur in contact sports.
They may occur during a tackle or in a one on one contest compared to a more traditional ankle sprain, which can occur simply by stepping on an uneven surface and rolling over on your ankle. Usually you need the traditional action of rolling your ankle combined with a load coming down across the ankle at the same time.
Football codes, such as rugby for example often involve tackling by multiple players. Last year in the AFL season we observed shortened and very ‘packy’ defensive games that increased the number of tackles performed per game. Hence the reason why I think we observed more ankle syndesmosis injuries.
There are different severities of syndesmosis related injuries. However, due to the overall influence this injury has on the ankles structural stability and function, they often need greater and longer intervention, sometimes requiring surgery.
A diagnosis can usually made in the clinic after observing typical clinical signs and symptoms and performing some stress testing to the affected ligaments.
Syndesmosis injuries are not always clearly identified on X-ray. More extensive scans such MRI and/or dynamic CT scans assist in a more rapid diagnosis and understanding of the injury severity and possible need for surgery.
Management
Initial acute management aims to offload and protect the injured tissues at all costs! A moon boot and crutches prevents any movement at the ankle and avoids placing any weight through the foot and ankle. Our Pro Ice machine is very effective at reducing initial swelling.
A mild syndesmosis ligament tear will require a period of immobilisation followed by a progressive rehabilitation plan to restore strength, balance and dynamic function of the foot and ankle. A player can take up 8 to 12 weeks to fully recover. In AFL a player may have sustained weakness in their ankle when kicking the football.
For more severe injuries, surgery is generally recommended. In these instances, conservative management may not be enough to address structural widening between the two shin bones or the overall ankle stability.
Surgical Management
There are a range of different surgical options to repair a syndesmosis injury depending on its severity. In some cases, there may also be a bone fracture due to the nature of the injury. Surgery may be required to repair any fractures that have occurred while also stabilizing the two shin bones. In the X-ray and image below you can see a common approach to repair a syndesmosis injury. Often screws and plates are used to realign the bones and offer structural stability to the joint longer term.
More recently an exciting new technique called ‘Tight rope” surgery has been developed. This technique is not widely performed. This type of surgery is less invasive, provides greater stability and requires less lengthy rehabilitation times of often less than 6 weeks. Tom Liberatore and Joel Selwood were examples of this in seasons 2016 and 2017, enabling them to return just before their respective final series.
Post-surgical rehab
There are generally 3 phases to post-surgical rehabilitation. This process is very individualised and will vary for each person. Below is a very general guide on the rehabilitation involved with surgical repair of syndesmosis injury. Obviously, this is not an exact time frame for everyone. Each person’s recovery and rehabilitation will be monitored closely to ensure the person continues to build up function and overall body conditioning specific to their given sport or activity.
Phase 1: (Week 1-6) – Recovery Phase:
Non-weight bearing and recovery with moon boot and crutches before progressing to slowly graduated weight bearing. This is often assisted with crutches, before moon boot is used alone. Rehab will include trying to ensure minimal loss of condition throughout the rest of the body where possible.
Phase 2: (Week 6-10):
General mobilisation and initial resistance exercises. The aim is to build load bearing stress, such as walking loads, functional balance stresses and muscles strengthening to the leg and ankle during this period.
Phase 3: (Week 10 onwards):
Progressing to dynamic types of exercises. This might include jogging and running loads. Hopping or jump to land exercises. Ideally this would progress to more varied movement patterns for agility and increased ankle stress. The aim is to build up load on the body and injury site to mimic sport specific movements, thus facilitate return to sport.
I hope you enjoyed and gained some further insight into syndesmosis injuries. Please keep your eye out for future posts as we explore common foot and ankle. Please feel free to like us on Facebook and Instagram so you will continue to be alerted to new content we post.
FARC specialises in post-surgical rehabilitation for all your lower leg, foot and ankle injuries